Top five Medicaid budget pressures for fiscal year 2025
As Medicaid programs move toward their new normal following unwinding, it’s worth taking a look at budget pressures facing states and territories in 2025.
Due to high tax revenues and federal pandemic assistance, the economic profile of state budgets remained relatively strong over the past few years. However, many state budget decisions will be more challenging as federal pandemic assistance expires and tax revenues decline. These factors ultimately impact the Medicaid program, as it is on average about 30 percent of total state spending in fiscal year 2023. State fiscal leaders are considering how external factors such as high-cost drugs, workforce shortages, and demographic changes will influence the budget and are implementing strategies to control spending and to ensure sustainability of the program and benefits.
So, let’s look at the top five Medicaid budget pressures for this year and what it means for Medicaid in ensuring millions of people live their healthiest lives.
But first, how did we get here?
When the COVID-19 pandemic hit in 2020, the U.S. rapidly plunged into a recession. The gross domestic product in Q2 2020 dropped by more than 30 percent from the preceding quarter, and millions of people lost their jobs. However, due to swift local, state, and federal relief, along with larger dynamics in the financial system, the U.S. economy quickly bounced back.
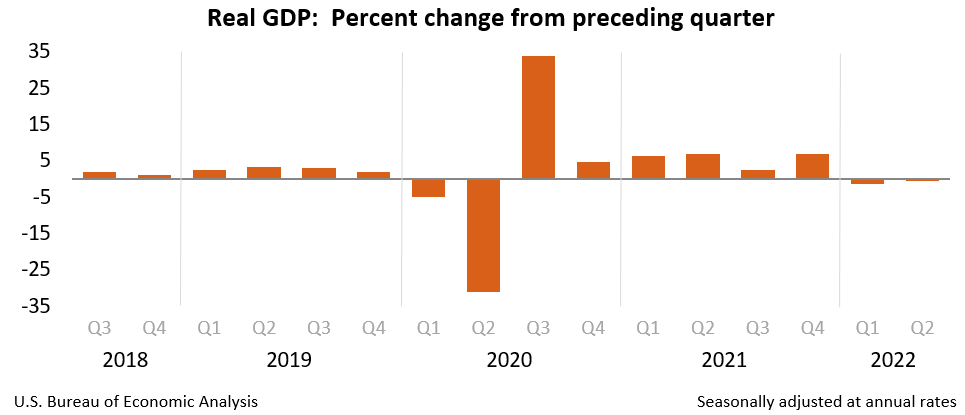
The U.S. Bureau of Economic Analysis shows the realities of changes to gross domestic product through the pandemic.
Because of higher-than-expected tax revenue, along with an influx in federal funds, the state of state budgets remained strong throughout the public health emergency (PHE). For instance, while fiscal year 2022 marked the highest year-over-year increase (16 percent) in general fund spending for over 40 years, states experienced three consecutive years of revenue surpluses.
However, we are already seeing those dynamics around strong state budgets start to shift. With the decline in federal funds, inflationary pressures, and enacted tax cuts, we are entering an era where state budgets will be much more influenced by outside pressures. For example, in fiscal year 2024, states will collect $13 billion dollars less in taxes, and consequentially, state budget officers are projecting a 1.8 percent decline in general funds revenue in fiscal year 2024.
Why should we care about Medicaid’s budget pressures?
So, as we transition into this new era of state budgets that won’t be as strong as they’ve been in the past several years, why is it important to consider Medicaid’s budget pressures?
Well, Medicaid produces a considerable amount of federal funding (i.e., FMAP) to cover health-related services. Every state dollar spent on Medicaid, yields anywhere between $1.00-$3.33 of federal funds depending on the state’s per capita income. And because Medicaid is an entitlement program, there is generally no cap for this federal funding. This means that, often, states will leverage Medicaid and the associated federal funding, whenever possible.
**It should be noted that financing to yield federal funds differs for the territories than it does for states.
All this to say is whether you count it by the state’s general funds, the federal fund expenditures, or the total expenditures, Medicaid makes up a large part of a state’s budget. Notably, in FY 2023, total Medicaid spending grew by 9.1 percent and that spending accounted for:
- 29.6 percent of total state spending, which is the single largest component of total state expenditures; and
- 18 percent of general fund spending, which is the second largest category of spending after K-12 education.
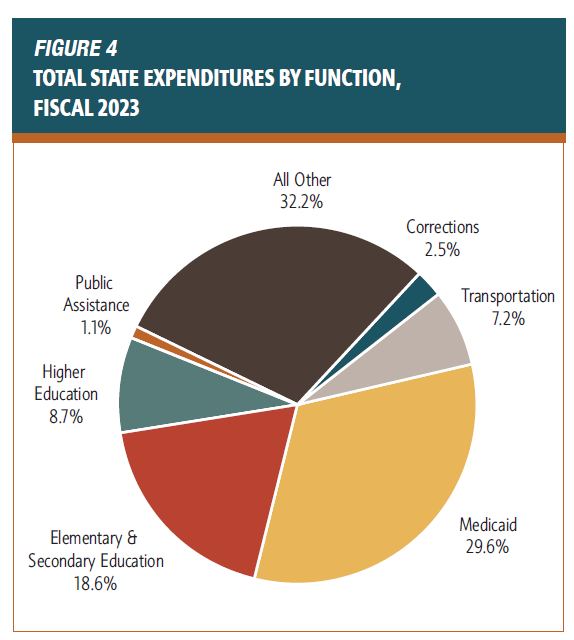
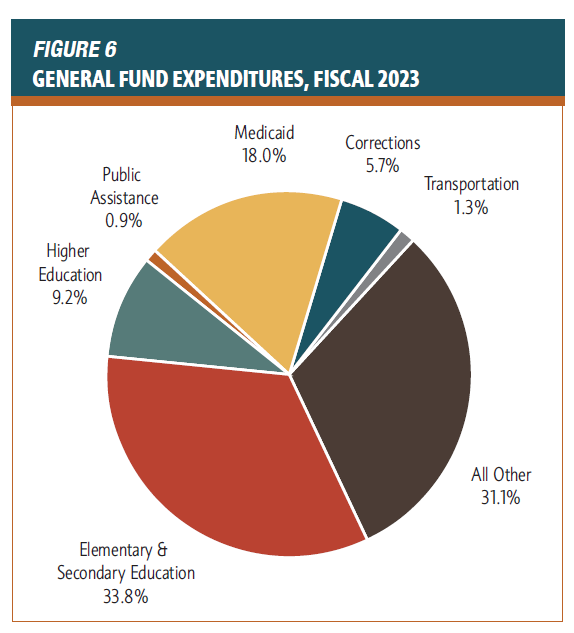
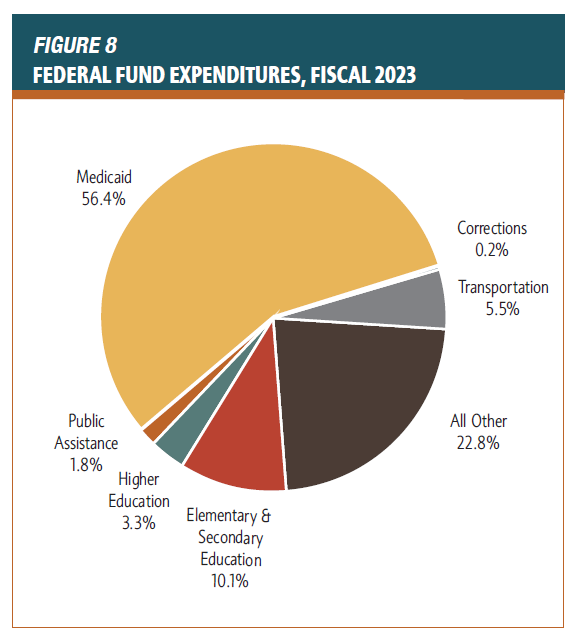
The National Association of State Budget Officers 2023 state expenditure report shows state expenditures by function, from the general fund and from federal funds.
That means that external factors (e.g., healthcare workforce shortages, inflation, changes in enrollment) can pressure the Medicaid budget. If these pressures reach a tipping point, it can result in cuts to the Medicaid program (e.g., limiting services, cutting reimbursement rates), or even impact the larger state budget. This is why sustainability is so important for the program, and we know state fiscal leaders are investing in an array of different sustainability strategies (e.g., investing in health-related social needs, primary care, preventative care, etc.) to prevent the program from reaching this type of tipping point.
Top 5 Medicaid Budget Pressures
Similar to state budget dynamics more broadly, Medicaid budgets will be tighter next fiscal year. For instance, we are seeing a more considerable rise in state fund spending for the program in fiscal year 2023 (16.6 percent) compared to fiscal year 2022 (5.4 percent), exemplifying how the program has started to impact the state general fund. So, let’s take a look at the top five biggest Medicaid budget pressure this next fiscal year, and it what it means for Medicaid and the overall state budget.
1. Unwinding: Sunsetting federal funding and uncertainty in enrollment projections
The unwinding, which is the nationwide mandate to redetermine eligibility for the 90-million Medicaid members who retained Medicaid coverage during the COVID-19 public health emergency, has been nearly all-consuming for Medicaid agencies this past year. Medicaid leaders have been working tirelessly to ensure that eligible individuals retain their Medicaid coverage, while they complete a three-year backlog of eligibility renewals. Unwinding has considerable fiscal impacts, and it’s driven primarily by 1) the reduction of enhanced FMAP associated with the public health emergency (PHE) and 2) the uncertainty associated with Medicaid enrollment.
Sunset of the enhanced FMAP associated with the PHE. Throughout the public health emergency, Medicaid agencies received a 6.2 percentage point increase in their FMAP for preserving the eligibility of everyone served by the program (i.e., continuous eligibility requirement) under the Families First Coronavirus Response Act (FFCRA). The Federal Funds Information for States estimates that this enhanced FMAP yielded more $119 billion to states through March 2023. The 2023 Consolidated Appropriations Act established the phasedown of the enhanced FMAP, which was completely sunset at the end of last year (2023).
Phasedown of Enhanced FMAP
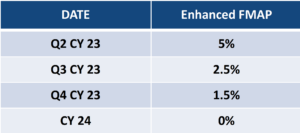
The CBO projects that in fiscal 2024, states will receive $58 billion less in federal Medicaid outlays than they did in 2023, and as a result, state spending on Medicaid will increase by 17.2% in FY 2024.
The uncertainty associated with projecting Medicaid enrollment pressures state budgets. Extended timelines, churn, new individuals enrolling on the program, and changes to eligibility policy ultimately impact the uncertainty associated with Medicaid enrollment projections next fiscal year. Enrollment forecasting can be incredibly difficult because there are no real economic indicators (e.g., unemployment rate) that can accurately predict Medicaid enrollment, so, fiscal leaders typically use historical data to project Medicaid enrollment. In unprecedented times, such as during unwinding, historical data may not be as accurate of an indicator for future enrollment as it was during more normal times.
During the PHE, Medicaid enrollment peaked at over 90-million individuals, and as unwinding continues Medicaid enrollment will continue to be higher than pre-pandemic levels. According to KFF analysis of CMS monthly reporting data, over 29 million eligibility renewals remain as of April 19, 2024. What will be the outcome of those renewals?
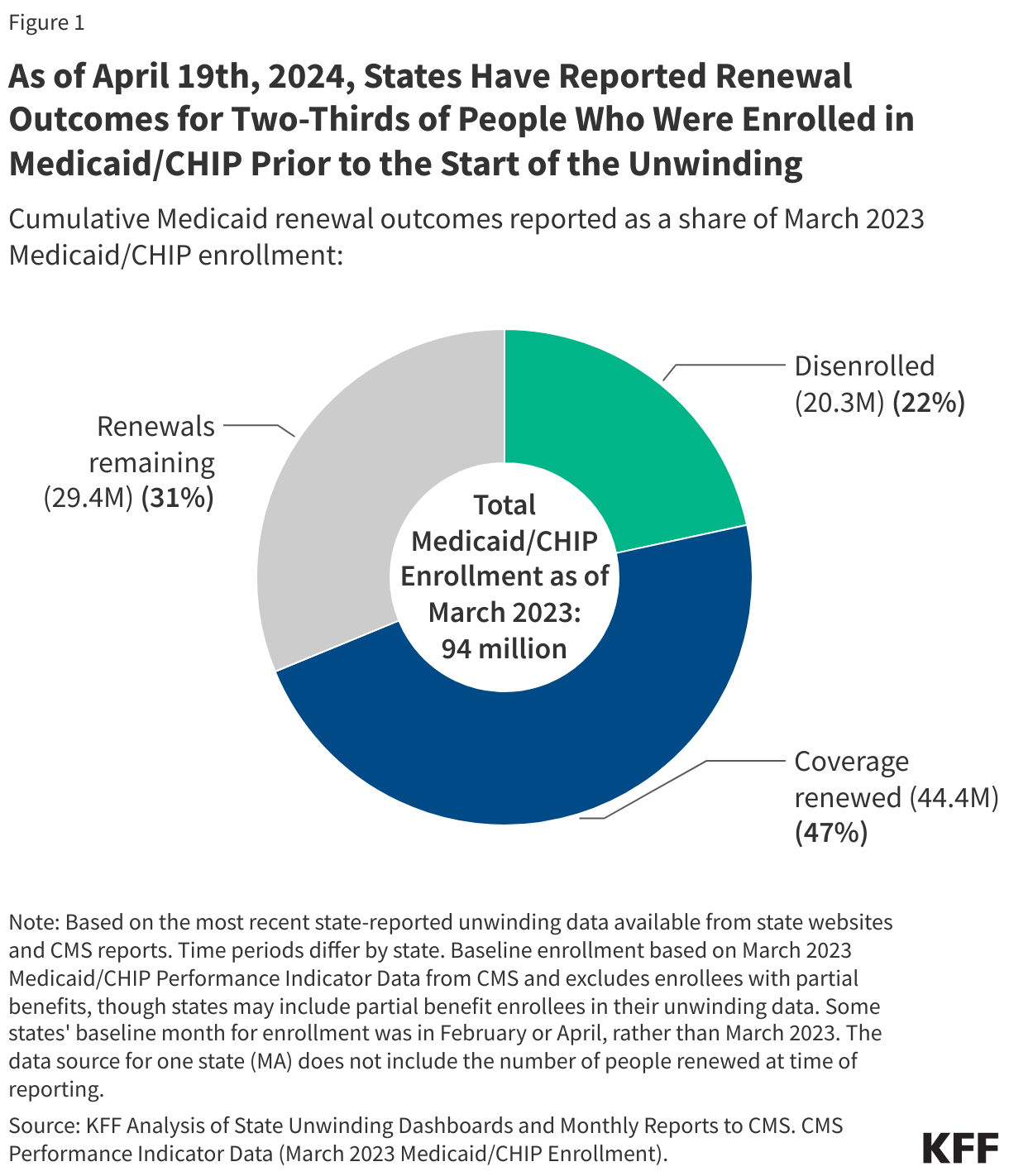
KFF’s enrollment and unwinding tracker overview as of April 19, 2024.
Given the backlog of eligibility renewals remaining, we are hearing that many Medicaid agencies will need to extend their unwinding timelines, so, Medicaid enrollment will continue to be higher than pre-pandemic levels. Even after a Medicaid agency completes the backlog of eligibility renewals, we think that folks should expect enrollment to be inflated for months, if not years, as folks churn on and off the program.
**Churn is when an individual is disenrolled from the Medicaid program and cycles back on the program shortly thereafter.
Before the unwinding, people churned on and off the program quite frequently. In 2018, 36 percent of people who lost Medicaid coverage, re-enrolled within 12 months. We are still learning more about how unwinding may impact churn rates, creating more uncertainty around enrollment projections. It’s hard to say when we will reach a steady state in enrollment, and these factors continue to complicate forecasting.
In addition to churn, enrollment remains open to new applicants throughout unwinding. In fact, due to the mass education and communication campaigns around unwinding, we are seeing higher than expected levels of new individuals and families applying for the program. Finally, because states and the federal government amended Medicaid eligibility policy in the last few years (e.g., postpartum extension, 12-month continuous enrollment for children), base-level Medicaid enrollment should be higher than it was before the PHE.
The convergence of these factors will keep Medicaid enrollment elevated well beyond the completion of unwinding activities. It is important to remember that disenrollments as a result of Medicaid unwinding does not equate to the net decrease in overall Medicaid enrollment. Because this is the first time the country has completed a three-year backlog of Medicaid eligibility renewals in a single year, there is a lack of data to project enrollment with certainty.
2. Prescription Drugs: Obesity-related medications and curative sickle cell treatments
Costs associated with prescription drugs play an increasing role in pressuring Medicaid budgets. This year, two treatments in particular (GLP-1 inhibitors and the new class of curative sickle cell therapeutics) may increase spending in the Medicaid program.
GLP-1 inhibitors are obesity-related medications (e.g., Ozempic, Wegovy) that can support weight-loss, treat diabetes, and/or heart disease, depending on the prescription. Generally, states do not have to cover this class of prescription drugs under the Medicaid Drug Rebate Program, however, there has been considerable interest in covering GLP-1 inhibitors because of their potential to improve health outcomes and save costs in the long-term. For instance, access to GLP-1 inhibitors could prevent chronic conditions, hospital visits, and other acute care. However, given the realities of churn and access to these prescription drugs, that return on investment and improved health outcomes are not always immediately realized. It’s too early to understand the fiscal and health outcomes associated with covering these prescription drugs, and it is an item that we value further research.
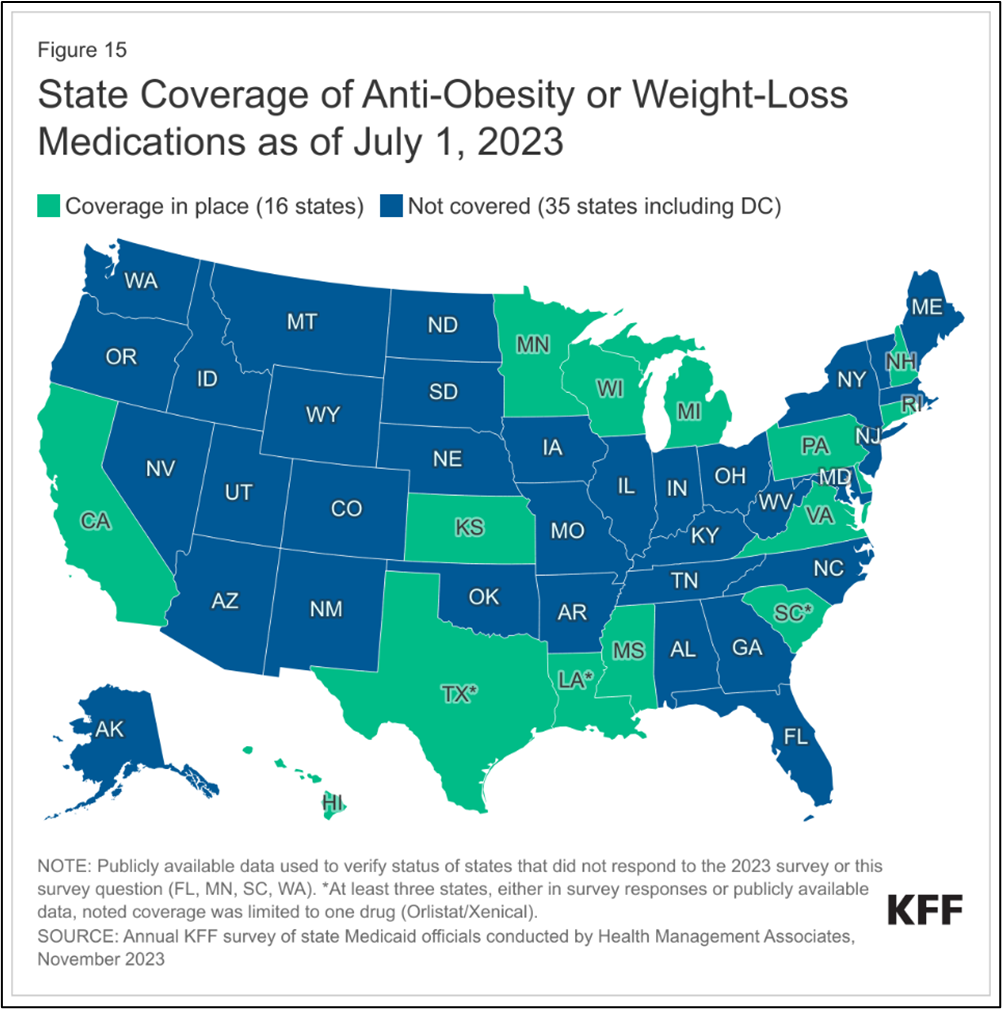
State reporting on anti-obesity drug coverage from KFF as of July, 2023.
While it’s estimated these prescription drugs cost $900 per prescription before rebate, utilization is the driving force for costs. More than two out of five U.S. adults aged 20 or over are obese. Partnership across financial and clinical leadership has been vital to understand utilization and utilization management to ensure access to these treatments, improve health outcomes, and have a comprehensive cost containment strategy in place.
The new class of curative sickle cell therapeutics, unlike GLP-1 inhibitors, must be covered under the Medicaid Drug Rebate Program. Estimates vary, but over 50,000 people nationwide who are served by Medicaid have sickle cell. They are predominantly Black (67 percent), aged 21 to 45 (39 percent) and live in Southern and Mid-Atlantic states.
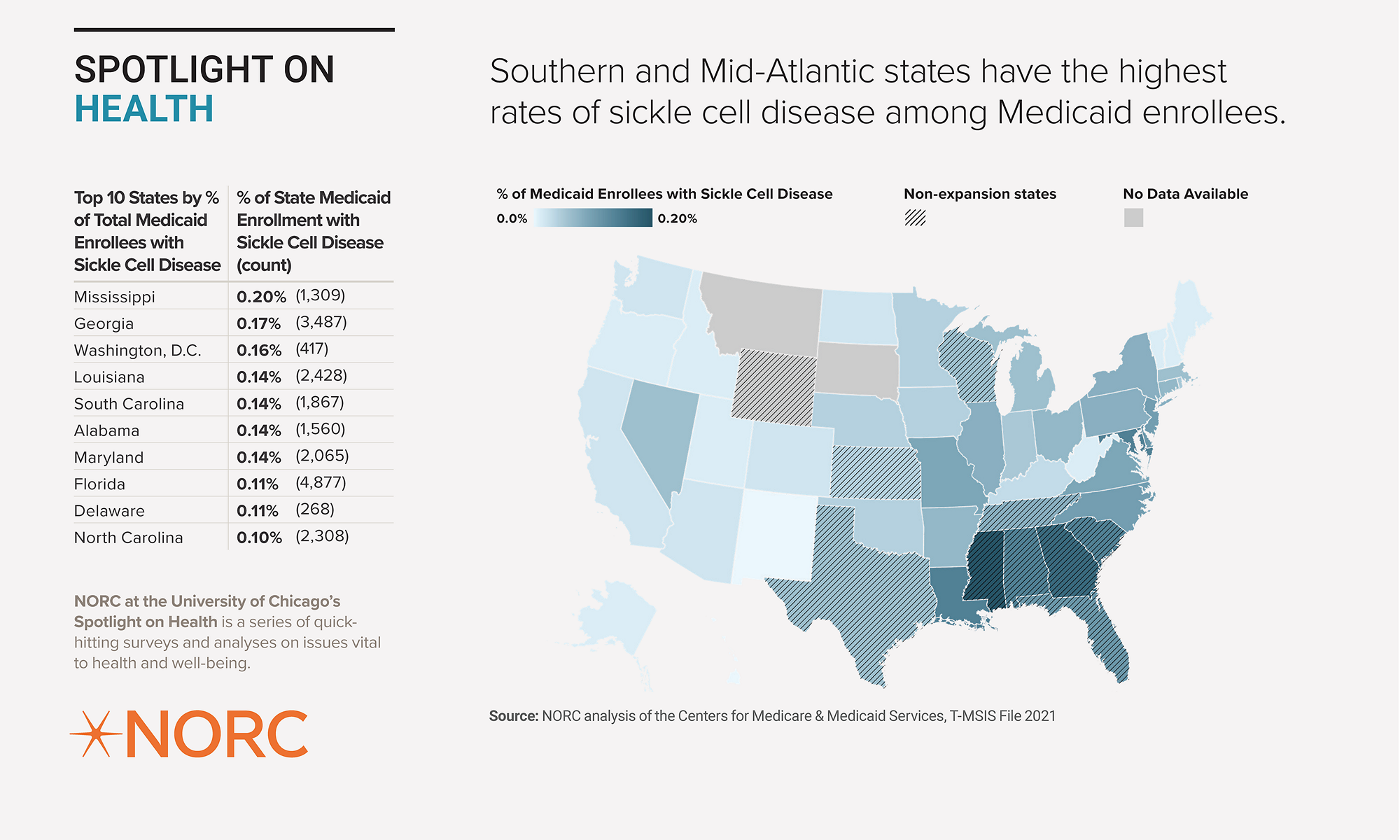
NORC data on the intersection of Medicaid members and sickle cell diagnosis.
These treatments are coming to market at $2.2 million (Casegevy by Vertex) and $3.1 million (Lyfgenia by Bluebirdbio) per person, which is similar, if not more than the disease-related medical expenses accrued over a single lifetime. Ultimately, this means that from a budgetary perspective, instead of paying for treatment over several decades, Medicaid would generally pay for a given treatment in a single budget cycle and potentially yield savings over several decades. Therefore, high-cost drugs introduce a certain level of budget volatility, and we’ve seen Medicaid agencies leverage high-cost drug pools, risk corridors, and other financial mechanisms to account for the fiscal risks associated with inaccurate utilization projections. In addition, the Center for Medicare, Medicaid Services’ Innovation Center recently established a payment model around cell and gene therapies, which will first focus on covering these new sickle cell therapeutics to support states covering the treatment and associated services.
However, given the clinical risks associated with the treatment, the limited provider pool that can administer these treatments, and the fact that the treatment regimen essentially requires an individual to live at the hospital for several months, we think that Medicaid will cover very few individuals for these treatments in the first few years or so. Ultimately, utilization will really be unique to each state, based on patients, providers, and other stakeholders.
While this discussion is focused on sickle cell, the FDA is currently reviewing Phase III applications for approximately 45 and 61 new cell and gene therapeutics for adults and children respectively. This suggests that Medicaid will continue to grapple with coverage policy for high-cost gene therapies. To learn more about how these therapeutics intersect with Medicaid, check out NAMD’s blog: Cell and Gene Therapies: Excitement tempered by reality.
3. Long-term Care: federal fiscal cliff and long-term demographic changes
Long-term care will have immediate and long-term impacts on Medicaid budgets. Immediate budget impacts are primarily influenced by the federal fiscal cliff associated with investments made for home and community-based services. In the long-term, demographic changes and a growing population of older adults will balloon long-term care spending in the Medicaid program.
Enhanced federal investments into home and community-based services are set to expire next year. In response to the COVID-19 pandemic, the federal government (i.e., Section 9817 of the American Rescue Plan) disbursed unprecedented levels of one-time spending to rebalance long-term care away from nursing facilities and towards home and community-based services (HCBS). Of course, efforts around rebalancing have long predated these investments with disability rights advocates, family members, and state and federal policymakers pushing for greater access to community-based care for years. In every year since 2013, Medicaid spending on HCBS outpaced spending on institutional care, demonstrating the shift in the long-term care delivery system in recent decades.
While some states initiated project-based work through American Rescue Plan funding, nearly all states used a plurality of these investments on provider payment initiatives to stabilize the direct care workforce. These federal funds are set to expire on March 31, 2025, for all but three states, and states will need to decide whether to continue those home and community-based investment, including pay increases for direct care workers, without that enhanced federal subsidy that was provided by the American Rescue Plan.
In the long term, as the single largest payer of long-term care, Medicaid will have to grapple with costs associated with a growing population of older adults that will require home and community-based services and/or nursing facility care in their later years of life.
Approximately 33 million or 1 in 10 Americans are between 65-74 years old. That is an over 50 percent increase from 2010. In the next one to two decades, this group of individuals will likely require some level of long-term services and supports. And while only a small subset of them will be covered by Medicaid, increases in enrollment for this population will continue to pressure the Medicaid budget. For instance, older adults and people with disabilities, together, make up 22 percent of the total Medicaid membership yet, they account for over half of the total expenditures in the program.
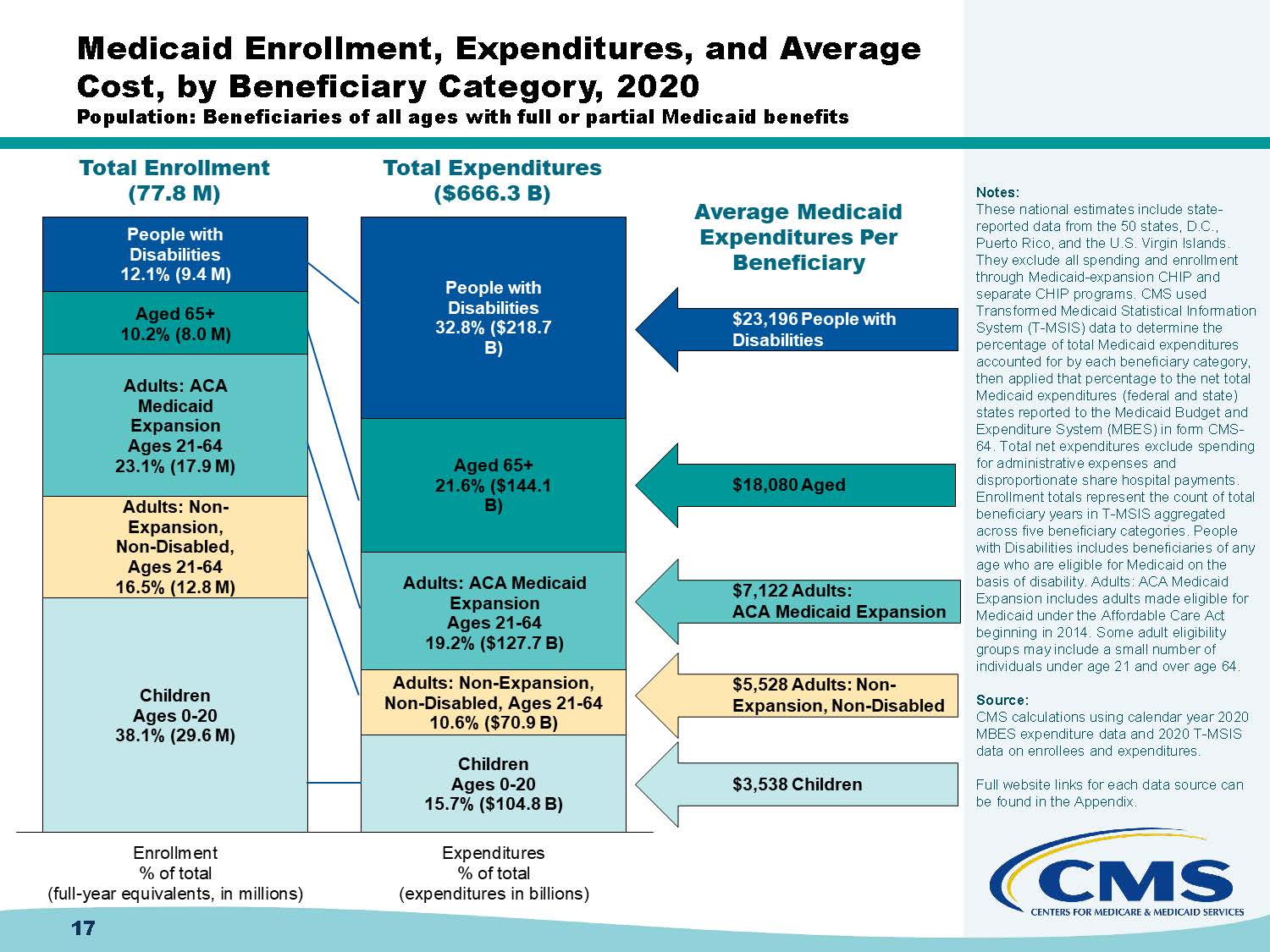
CMS outlines the data around Medicaid enrollment, expenditures and average cost by member type in 2020.
Demographic changes impact Medicaid budgets now, and the magnitude of impact will only increase in the next few decades. The convergence of demand, rebalancing, and pricing will ultimately catalyze us to rethink how deliver and cover long-term care in our country.
4. Provider Rates: Workforce shortages and Inflation
Critical healthcare workforce shortages compounded by inflation will pressure Medicaid budgets through provider rate increases next fiscal year. In order to attract and retain the healthcare workforce needed to address shortages, states will have to invest in the education and training pipeline as well as rates, wages, and fringe benefits for providers who serve Medicaid members.
- The Bureau of Labor Statistics estimates a shortage of nearly 200,000 nurses by 2031
- The AAMC estimates a shortage of between 18,000 – 48,000 primary care physicians
- PHI estimates the direct care workforce will fall short of demand by nearly 9 million jobs from 2020 to 2030
A robust healthcare workforce is a vital component to ensure access to care, and according to Health and Human Services currently millions of Americans live in a health professional shortage area (HPSA). To support retention of health care practitioners and sustain safety-net providers with thin margins, Medicaid agencies have been increasing provider rates.
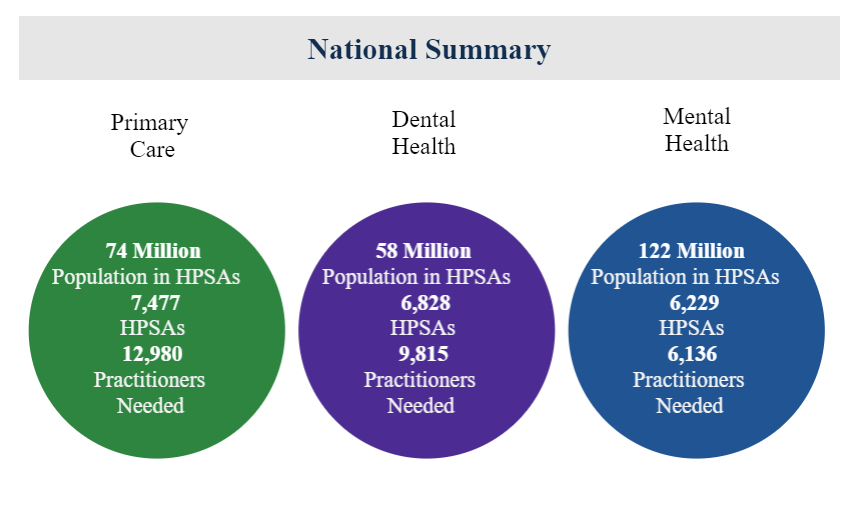
Health Resources and Services Administration data on the realities of the health care workforce shortage.
And larger labor market dynamics contribute to upward pressure on wages. For example, home health agencies and nursing facilities must pay more to compete with other sectors (e.g., fast food, retail, etc.) that employ low-wage workers. As a reminder, enhanced federal funds for home and community-based services will expire in May 2025, so states will take on a bigger share of the costs associated with sustaining those rate increases.
Inflation is also putting pressure on rates. While overall inflation has largely tempered in recent months, medical inflation typically lags several months behind regular inflation. In addition, cost increases in non-medical sectors (e.g., energy, food, etc.) also impact health care.
We know that many state legislatures are considering provider rate increases this session. However, with limited funds, states will need to prioritize investments into parts of the healthcare delivery system where Medicaid has an outsized role (e.g., behavioral health, maternal health, long-term care). For example, we know some states are conducting comprehensive bench-marking studies, which can be incredibly complicated and labor intensive, to better allocate limited resources around provider rates.
5. Administrative budget: IT systems and Human Resources
While relatively small compared to the overall Medicaid budget, administrative budgets are increasing in size to pay for the IT systems and human resources necessary to effectively meet the commitments of the program. For instance, to comply with longstanding federal eligibility rules as well as new federal requirements, Medicaid will require significant investments into IT systems. A few examples of federal requirements that need IT investments include:
- Consolidated Appropriations Act requirements for justice-involved youth (effective January 1, 2025)
- Managed care and access rules (finalized April 2024)
- Eligibility compliance plans (date unknown) and new eligibility final rule (finalized March 2024)
- Re-programming systems after temporary unwinding system changes
In addition, Medicaid programs will need staff and contractor resources to meet these federal requirements and administer daily operations. However, ongoing challenges around recruitment and retention in state government, especially for highly paid skills in the private sector, will pressure the Medicaid administrative budget in salaries. Finally, states still face continued need for extra eligibility staff and contractor resources to resolve the backlog of eligibility renewals associated with unwinding.
While this discussion has primarily focused on the array of federal requirements coming down the pike in the next few months and years, it’s notable that administrative budgets expand to address unforeseen issues and emergencies impacting Medicaid members and providers. For example, in the past few weeks, Medicaid agencies across the nation have had to rapidly mobilize and implement innovative solutions to ensure millions of Medicaid members have access to critical healthcare services in response to a major cyberattack on one of the nation’s largest healthcare digital clearinghouses, Change Healthcare. All this to say is that new programs and requirements in the Medicaid program require commensurate administrative resources (e.g., IT upgrades, staff, etc.) to fully operationalize them.
So, what does this all mean?
While budgets remain largely healthy across states, this may be the first time in a few years, where Medicaid budget pressures may be more likely to influence the overall state budget. To prevent impacts that would require the program to cut costs (e.g., cut provider rates, cut services), Medicaid and budget leaders are working to accurately inform projections and state budgets. For instance, some states use a consensus budget process to ensure key policy and finance leaders inform the budget. Other states developed specific Medicaid rainy day funds to ameliorate the member-facing impacts of a Medicaid budget shortfall, which are much easier to access than the general rainy-day fund. We are also seeing states control cost trends through strategies such as health-related social needs initiatives (e.g., housing, food, employment, etc.), investments into primary care and preventive care, and improvements in maternal health and behavioral health.
We’ll continue to keep tabs on the state of state budgets as changes in federal policy, high-cost drugs, and the economy increase Medicaid state spending.
This overview was created in partnership with the National Association of State Budget Officers. Their annual report on State Budget Expenditures is an invaluable resource for understanding Medicaid and its impact on state and territorial budgets. You can visit NASBO and see all their resources.
Related resources
NAMD Comments on Medicare’s Proposed Coverage Determination for Alzheimer’s Drug
NAMD Joins State Associations in Requesting that Congress and the Administration Help States Prepare for the End of the Public Health Emergency
Stay Informed
Drop us your email and we’ll keep you up-to-date on Medicaid issues.