Why did they do it that way? Eligibility policy
Check out NAMD’s latest issue brief to learn more about Medicaid eligibility policy.
Who is eligible for Medicaid?
As of June 2023, Medicaid covered approximately 93 million people, representing one of the largest health insurance programs in the country. Unlike other health insurance programs that observe annual open enrollment periods, individuals who are eligible to enroll in Medicaid can do so at any time. But who is eligible to enroll in Medicaid? All states and territories cover the same mandatory eligibility groups, including low-income families, pregnant people, and people with disabilities. Outside of these mandatory groups, states and territories have flexibility to tailor eligibility policy to meet local priorities and constraints, resulting in significant variation across the 56 Medicaid programs in the states, US territories, and the District of Columbia.
Currently, there at least 35 distinct pathways to Medicaid and CHIP eligibility listed under Title XIX and Title XXI of the Social Security Act. These categories are generally defined by financial factors, like income and assets, and non-financial factors, like disability status, age, citizenship, and pregnancy. Under federal law, states1 are required to cover certain “mandatory” eligibility groups, including low-income children, low-income pregnant people, certain parents and caregivers, and individuals receiving Supplemental Security Income. Other eligibility groups – including people with high medical expenses, people who need home and community-based long-term care services, and low-income adults who do not have children – are at state option. States also have authority to elect to cover people at higher income ranges and, for HCBS, to cover them on a population-specific basis that is otherwise not permitted under Medicaid state plans.
As in other areas of Medicaid policy, federal law sets a “floor” of mandatory eligibility groups and processes. Some states and territories, due to policy priorities and/or fiscal constraints, have chosen to focus on these core mandatory groups. Others have chosen to cover additional optional eligibility groups, to cover mandatory groups at higher income thresholds, or to use waivers to test new eligibility frameworks (e.g., tying Medicaid eligibility to employment or community engagement requirements). This leads to substantial variability across states and territories in who is eligible for Medicaid.
How did we get to this point?
Medicaid eligibility has expanded incrementally since the program’s creation in 1965, often in response to issue-based advocacy. Until the 1980s, Medicaid existed as safety net health coverage for older people and people with disabilities who were receiving payments through the Supplemental Security Income program (SSI) and for low-income families receiving cash assistance through Aid for Families with Dependent Children (AFDC) programs. During this time, Medicaid eligibility policy was run out of the state/territory agencies who oversaw SSI and AFDC programs, allowing Medicaid agencies to focus primarily on benefits and service delivery, not eligibility. This history has important impacts on how Medicaid agencies are structured today.
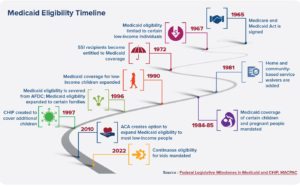
In the 1980s, Congress began to expand Medicaid coverage to additional groups, including individuals who met the requirements for AFDC or SSI but weren’t actually enrolled in these programs, pregnant women and infants, children under age six, and children under age 19. When AFDC was replaced with Temporary Assistance for Needy Families (TANF) in 1996, Congress required states to cover certain low-income families, with the option to cover families with higher incomes.
In 2010, the Affordable Care Act (ACA) enacted the largest changes in Medicaid eligibility policy since the program’s inception by establishing new coverage groups, setting new requirements for how Medicaid applications and redeterminations are processed , and shifting to the use of Modified Adjusted Gross Income (MAGI) as a method for calculating income. Notably, the ACA expanded eligibility to low-income, childless adults for the first time. The subsequent 2012 Supreme Court decision in National Federation of Independent Business v. Sebelius made this expansion of Medicaid eligibility optional.
How do Medicaid eligibility processes work?
Not only does federal law require certain populations to be covered, it also sets minimum standards for how states and territories process Medicaid applications. For example, all states and territories are required to use a single streamlined application, accept applications through telephone, mail, internet, or in person, and process Medicaid applications within 45 days.
Federal law also sets minimum standards for how states must conduct redeterminations of Medicaid eligibility. Generally, federal law requires Medicaid members to renew their eligibility approximately every 12 months. Under the Affordable Care Act, states and territories must first use available data sources to attempt to automatically renew someone’s coverage (also called an ex parte or administrative renewal). If the individual’s coverage cannot be automatically renewed, the Medicaid member must complete a renewal form that is sent to them by the Medicaid agency. If the Medicaid member does not return this renewal form, or if the member does return the form but no longer meets eligibility requirements, the agency is required to end their Medicaid coverage and notify them about (and, in some cases, help them transition to) other forms of health insurance.
Medicaid members are also proactively required to report “changes in circumstances” that may impact their eligibility. For example, if an adult is eligible for Medicaid on the basis of their income and gets a new job with higher pay, they would need to report that change to the Medicaid agency. The agency would then evaluate if the individual still meets eligibility criteria for their current, or another, eligibility group.

Federal regulations establish these basic components of eligibility: application, renewal, and changes in circumstances. Congress can, however, change these eligibility standards by amending federal Medicaid laws. For example, Medicaid agencies are newly required to provide 12 months of continuous eligibility for children starting January 1, 2024. This means that children who are determined eligible for Medicaid will be entitled to 12 months of coverage, even if their parents’ income or other circumstances change. Congress can also change eligibility requirements on a time-limited basis; during the COVID-19 federal public health emergency declaration, for example, Congress created a “continuous coverage” requirement to preserve access to care.
Beyond these requirements, states and territories have significant flexibility in setting eligibility policy for their programs. States and territories can set income limits for different eligibility categories, disregard certain income or assets, and use eligibility findings from other programs like SNAP and TANF to streamline enrollment in Medicaid. Some states have also applied for federal waivers to extend continuous eligibility to adults, lengthen the period of continuous eligibility for children, or make other changes to eligibility processes for specific groups.
How do states make decisions around eligibility policy?
Why might a Medicaid program choose to cover or not cover certain eligibility groups? One framework for understanding Medicaid policymaking is examining priorities and constraints. A state policymaker – such as a governor, legislator, or Medicaid Director – may have certain policy priorities around Medicaid eligibility. For example, many states have elected to expand Medicaid eligibility to 12 months postpartum, with the goal of improving maternal health outcomes. Similarly, many states have adopted optional pathways to expand Medicaid eligibility for people with disabilities.
Policymakers must weigh these policy priorities against constraints. The most relevant constraint in eligibility policy is often budget; more expansive eligibility policies lead to higher program enrollment, which can result in increased cost. But policymakers must also consider other constraints, like the Medicaid agency’s administrative capacity, or the number of staff available to develop policy, process eligibility cases, and respond to member inquiries. Policymakers also need to consider the technical capabilities of their IT systems; many changes to eligibility policy require changes to the IT systems that manage eligibility and enrollment, and these changes can be costly and time-consuming. Finally, policymakers need to be mindful of federal eligibility regulations, which set guardrails on the types of eligibility policies states and territories may implement.
What operational factors impact eligibility?
In addition to making decisions around Medicaid eligibility policy, states and territories must also set up systems to manage the day-to-day operations of enrolling people in Medicaid and renewing their eligibility. Strong operational systems help ensure that Medicaid programs operate efficiently and that eligible people can easily enroll in Medicaid.

Agency Structure
As Medicaid has evolved over time, eligibility for the program has expanded substantially. Originally, Medicaid primarily served individuals eligible for SSI and AFDC. Because of this, Medicaid eligibility functions were historically run out of the human services agencies that oversaw SSI and AFDC.
In many states, this structure has persisted. In a 2021 survey, NAMD found that around a third of Medicaid agencies manage their eligibility processes directly; in the remaining states, other human services agencies (such as those responsible for SNAP and TANF) may entirely or partially oversee Medicaid eligibility. Some states also have contracts with county or municipal governments, in which the county or municipality agrees to process Medicaid applications and renewals.
Having Medicaid eligibility functions managed by an outside agency can create challenging dynamics: even if the Medicaid Director is in charge of setting eligibility policy, they have less explicit authority to manage policy implementation and address emerging issues. Because eligibility processes can have big impacts on the experience of Medicaid members, the program budget, and access to services, it is essential to build strong working relationships between Medicaid and the agency overseeing eligibility policy.
Eligibility Workers
Eligibility workers are the primary point of contact for individuals who are seeking to enroll in Medicaid. Federal law requires that Medicaid eligibility be determined by an individual hired via a government civil service, merit selection process. This means that eligibility workers are state, county, or municipal employees.
Eligibility workers are responsible for collecting information, verifying information either through data matches or through documentation provided by the member, and determining eligibility. They do this for new applications, annual renewals, and when changes in circumstances are reported. Many times, these same workers are responsible for determining eligibility for other programs, including SNAP, TANF, and childcare assistance, which have different eligibility rules. Because of this, it can take weeks of training before a new eligibility worker can begin processing Medicaid applications or renewals, and it can take months or years for eligibility workers to gain expertise in the most complex areas of Medicaid policy. This can make it challenging for states and territories to quickly ramp up their capacity to handle an uptick in program participation, as occurred during the COVID-19 public health emergency.
Eligibility and Enrollment Systems
Medicaid eligibility and enrollment systems are a core component of how agencies process applications and renewals. These IT systems collate and synthesize data that is received from Medicaid members (through paper and electronic applications and renewal forms) and connect with other electronic data sources, such as SNAP data and Internal Revenue Service (IRS) data. These data connections allow states and territories to conduct automated eligibility checks, as required by the ACA. More broadly, eligibility and enrollment systems allow agencies to process applications, track when a member needs their annual redetermination, and send out renewal forms and notices.
Eligibility and enrollment systems vary widely across states and territories. While many states and territories contract with vendors to design, implement, and manage their eligibility and enrollment systems, others develop and operate their systems in-house. Systems also vary in their age, structure, functionality, and integration with other social service programs. For example, some states have connected their eligibility and enrollment systems to self-service portals, so that Medicaid members can take certain actions (like submitting required forms and documents) online. Many states and territories are currently undertaking efforts to modernize their eligibility and enrollment systems, which may improve the experience of Medicaid members and streamline administrative processes. Systems modernization efforts, however, can be extremely time-intensive and costly.
Medicaid members often receive other benefits, like SNAP, TANF, and childcare subsidies. Because of this overlap, many states have integrated eligibility and enrollment systems that are used to determine eligibility for a range of programs. Similarly, some states with state-based Marketplaces have developed systems that integrate eligibility for Medicaid and Marketplace plans. Integrated systems can streamline data-sharing between programs, reduce duplication of efforts for eligibility workers and Medicaid members, and help ensure individuals have access to all of the benefits for which they may be eligible. However, implementing systems changes can be more challenging in integrated systems, as changes to Medicaid eligibility rules may impact other programs.
How is Medicaid eligibility policy continuing to evolve?
Federal regulations establish the basic outline of Medicaid eligibility policy, including mandatory and optional eligibility groups and rules for how states process applications and renewals. Within these guardrails, states and territories have significant flexibility to design Medicaid eligibility policy, including which groups they cover.
Medicaid eligibility has expanded significantly since the program was created in 1965, with new eligibility groups and policy options added by Congress over time. We are continuing to see Medicaid eligibility policy evolve, with Congress newly requiring 12-month continuous eligibility for kids in 2024 and CMS proposing major new regulations that govern eligibility policy and processes.
Perhaps most significantly, Congress set a start date of April 1, 2023, for the end of the COVID-19 continuous coverage requirement and the initiation of redeterminations for all people on the Medicaid program at that point in time. This national Medicaid redetermination process – often called the “unwinding” – has brought unprecedented attention to Medicaid eligibility policy and operations. As part of the unwinding, many states are undertaking longer-term efforts to streamline eligibility processes and modernize their IT systems; these efforts are aimed at coming into permanent compliance with ACA-era regulations or otherwise improving Medicaid members’ ability to navigate the renewal process. Although the unwinding is slated to end in 2024, these efforts have the potential to improve Medicaid eligibility processes in the long-term, creating a smoother experience for individuals seeking to enroll in Medicaid and increasing the efficiency of state operations.
This resource was developed with support from The Commonwealth Fund, a national, private foundation based in New York City that supports independent research on health care issues and makes grants to improve health care practice and policy. The views presented here are those of the author and not necessarily those of The Commonwealth Fund, its directors, officers, or staff.
Related resources
Why Did They Do It That Way? Program Integrity
How eligibility may look different in this bridging year
Stay Informed
Drop us your email and we’ll keep you up-to-date on Medicaid issues.
