Q&A with Gary Smith: Leading Medicaid in the U.S. Virgin Islands
Gary Smith has served as Medicaid Director for the U.S. Virgin Islands for the past eight years. In this Q&A, he shares insights about leading a territory Medicaid program, the unique challenges territories face, and his work organizing the inaugural U.S. Territories Medicaid Enterprise Systems Summit.
Author
- Carly Sfregola
Gary Smith has served as Medicaid Director for the U.S. Virgin Islands for the past eight years. In this Q&A, he shares insights about leading a territory Medicaid program, the unique challenges territories face, and his work organizing the inaugural U.S. Territories Medicaid Enterprise Systems Summit.
Q: What motivated you to pursue a career in public service?
Helping people has always been a part of my family’s DNA. My maternal grandmother—anyone in the neighborhood could stop by her on a daily basis and get a meal. Saturday she would cook so many different meals, and everyone—uncles, aunts, cousins, friends, neighbors, and anyone that came by could get a plateful.
My mom is also a retired registered nurse, my dad began his career as a schoolteacher and then became a health care executive. I aspired to be a hospital administrator, but being the Medicaid director for the past 8 years has been very gratifying, to say the least. It’s something that my family raised me with—being taught to be nice to people and help people when you can.
Q: What is it like to lead a territory Medicaid program? What are the unique challenges territories face compared to states and how are they funded differently?
Our community is very small, and as the Medicaid director, I am accessible to the public at all times. I have folks walking through the building and they come and knock on my door: “Are you Mr. Smith, the Medicaid director?” Members call me directly on a daily basis.
Due to the small size of our program and staff, I get to be involved in most or all aspects of our program from a leadership perspective.
Our greatest challenge is funding. We manage limited budgets and still have to manage the expansive community health needs of our territory. We receive a fixed amount block grant model compared to the states where they have open-ended funding. Underfunding forces us to make very tough decisions on eligibility, benefits, and provider payments where we’re not able to pay providers timely.
Our health care infrastructure faces persistent gaps and challenges—hospitals operate with aging infrastructure and suffered major hurricane damage in 2017. Rebuilding and modernization have been slow. Specialty care facilities are sparse, forcing many of our citizens to travel off-island for advance treatment. Recruitment and retention of physicians, nurses, and specialists are difficult due to high cost of living, limited professional growth opportunities, and infrastructure challenges.

Q: The 2023 Congressional directive required the territories to develop comprehensive four-year strategic plans covering workforce, program integrity, systems development, and financing. Can you walk us through your approach to developing the USVI’s plan including the systems component?
This provided us with a very significant opportunity to shape our Medicaid program to be resilient, efficient, and improve our health care infrastructure. We started by building a project framework aligned with CMS’s expectations but also including our unique needs. The strategic plan is based on four pillars, Program Integrity, Medicaid Financing, Workforce Development, and Systems Modernization, and most important—disaster resilience.
In the Virgin Islands we were the first territory with a certified MMIS system, which was certified back in 2013. An MMIS system, or Medicaid Management Information System, is like the backbone of your program. Our approach focused on building capacity, automating workflows, and working towards making decisions based on data.
Right now on our radar is making sure our eligibility and enrollment system has a fully functional member portal and the implementation of provider enrollment application (PEA) which will streamline the provider enrollment process. We’re also working with our Office of Health Information Technology to implement a health information exchange and with our Department of Health to implement a universal data warehouse.
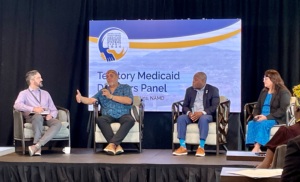
Q: You organized the inaugural U.S. Territories Medicaid Enterprise Systems (MESC) Summit. What inspired you to pull together this first-of-its-kind event, and what were the key breakthroughs or collaborations that emerged from bringing territory leaders together?
This was definitely a strategic but also a very personal initiative for me. At MESC 2023, CMS held a day and a half summit in Colorado with all the territories. In conversations with CMS, I said, “Hey, let’s have this summit in the Virgin Islands in 2024.”
We wanted to close longstanding gaps in our Medicaid systems and infrastructure across the territories. The conference was a platform for us to share our challenges but also realizing that each of us have our isolated issues and we needed to come together and have those discussions.
It became very apparent that we were all navigating these challenges in silos and reinventing the wheel when there already exists solutions—states already solved these issues. So being able to connect our territories with other Medicaid programs across the nation was crucial.
What has developed from that: we now have quarterly meetings with the territories and CMS, there’s more focused technical assistance for the territories. On the NAMD side, we stood up monthly territory meetings. There’s a lot more engagement now with our Pacific territories and CMS, and also with vendors.
Q: What advice would you give partners that want to work more closely with Medicaid?
If you’re a partner, whether you’re a provider, a vendor, an advocacy group, a university or community-based organization, working more closely with your Medicaid programs can be transformative. But it requires a deep understanding of our programs, understanding what the programs’ priorities are, what the constraints are, and what the culture is.
Cultural sensitivity is paramount. That is so important for you to understand our culture [in each territory] and making sure that you can align with that, but then also adapt and adjust, because our pace is not the pace in the states that you’re accustomed to or used to. It’s a different vibe.
Our low-income and vulnerable populations are different as well. Don’t sell your product first—try and understand what our needs are and what the issues are that we need to address. Start with the problem and not the product and appreciate the challenges and issues that we face.
Related resources
Building Trust One County Fair at a Time: Q&A with Kentucky’s Medicaid Director Lisa Lee
Q&A with Jen Strohecker: Leading Through Crisis and Closing Cracks in Care
Stay Informed
Drop us your email and we’ll keep you up-to-date on Medicaid issues.