CMS releases guidance on new required services for incarcerated young people
NAMD’s analysis of recent guidance on required services for young people who are returning from incarceration.
Author
- NAMD Staff
Focus Areas
Program Stream
In December 2022, Congress passed the Consolidated Appropriations Act (CAA) of 2023. The omnibus spending bill included several policies impacting the Medicaid program, including new requirements for how Medicaid and CHIP agencies provide services for young people who are incarcerated. Specifically, Section 5121 requires that Medicaid and CHIP agencies cover certain screening, diagnostic, and case management services for young people who are incarcerated and post-adjudication, with a compliance deadline of January 1, 2025. Section 5122 creates a new option for states to provide the full range of Medicaid and CHIP services to incarcerated young people who are being held pending disposition of charges.
In July 2024, CMS released guidance explaining what states and territories will need to do to meet this statutory requirement. What does the guidance say, and what will states and their correctional partners need to do by January 1, 2025? Read on for NAMD’s analysis.
What do states need to do by January 1, 2025?
By January 1, 2025, states will need to have an “internal operational plan” in place, containing the elements listed below. States will also need to submit certain Medicaid and CHIP State Plan Amendments (SPAs) with effective dates no later than January 1, 2025, to implement the Section 5121 requirements.
States’ internal operational plans must be in place no later than January 1, 2025. States are not required to submit these plans to CMS, except upon request. Internal operational plans must include the following elements:
- “Actions for establishing an operational system and updating the system as needed on an ongoing basis, to perform functions such as exchanging data with the carceral system;
- Procedures for Medicaid and CHIP eligibility, enrollment, applicable notifications, and claims processing;
- Processes to ensure the timeliest possible provision of screening and diagnostic services if they are not able to be covered beginning 30 days prior to release;
- Policies, procedures, and processes to ensure pre-release services do not effectuate delay of an individual’s release or lead to increased involvement in the juvenile and adult justice systems;
- New or updated written staff-level operational policies and procedures where workflows and processes are impacted by the new requirements;
- New or updated provider and beneficiary-level processes, procedures, policies, and systems related to accessing services such as case management, prior authorization, linkages with managed care plans, payment, claims processing, and data analysis, where these are impacted by the new requirements;
- Training, education, and outreach actions; and
- Integration with current Medicaid and CHIP operations, such as disaster planning and continuity of operations, hearings and appeals, beneficiary notices, record retention, and other operational activities associated with program administration.”
States will also need to submit the following SPAs:
- All states must submit a Medicaid SPA attesting “that the state has developed an internal operation plan, and in accordance with such plan, will provide coverage during the statutory pre- and post-release period of screening, diagnostic, and targeted case management services for eligible juveniles who are within 30 days of release post adjudication.”
- These SPAs must have an effective date no later than January 1, 2025, so they must be submitted no later than March 31, 2025.
- CMS will release a SPA template.
- Some states may need to submit a SPA authorizing coverage of certain screening, diagnostic, and/or targeted case management (TCM) benefits, including adding new targeted case management target groups.
- These SPAs must have an effective date no later than January 1, 2025.
- States that do not have an approved payment methodology for these services will need to submit a payment SPA.
- These SPAs must have an effective date no later than January 1, 2025, so they must be submitted no later than March 31, 2025.
- For CHIP, states must submit a SPA to effectuate coverage of the Section 5121 screening, diagnostic, and case management services. States must also submit a SPA complying with the eligibility policy changes.
- These SPAs must have an effective date no later than January 1, 2025, so they must be submitted no later than the end of the state fiscal year in which January 1, 2025, falls.
- CMS will release a SPA template.
What services do states need to provide?
Under Section 5121, states need to provide screening and diagnostic services to eligible juveniles in the 30 days prior to release (or not later than one week, or as soon as practicable, after release) and provide targeted case management services in the 30 days prior to release and for at least 30 days following release. CMS provides additional detail on what each of these service categories includes. Under the option in Section 5122, states would provide coverage of all mandatory and optional services that an eligible juvenile would otherwise be entitled to if not for their incarceration.
- Screening and diagnostic services: States must provide screening and diagnostic services in the 30 days prior to release (or not later than one week, or as soon as practicable, after release). In Medicaid, screening and diagnostic services include “any screenings and diagnostic services which meet reasonable standards of medical and dental practice, as determined by the state, or as otherwise indicated as medically necessary, in accordance with the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) requirements, including a behavioral health screening or diagnostic services.” In CHIP, they include “screening, diagnostic, and case management services otherwise available under the CHIP state plan (or waiver of such plan).”
- EPSDT only applies to individuals up to age 21. For eligible juveniles under age 21, states should cover EPSDT services as they would for young people who are not incarcerated. For individuals older than 21, states will need to use state-determined reasonable standards of medical and dental practice, including “screening services when they are medically necessary to determine existence of a physical or behavioral health illness or condition as well as diagnostic services when a screening service indicates the need for further evaluation and when such diagnostic services are otherwise medically necessary.”
- CMS notes that EPSDT screening services include immunizations.
- Targeted case management: States must provide targeted case management, including referrals to care, in the 30 days prior to release and for at least 30 days following release. In Medicaid, CMS uses the definition of targeted case management (TCM) at 42 C.F.R. § 440.169. States may need to submit a SPA to add a specific target group for eligible juveniles to their targeted case management benefit.
- CMS clarifies that Medicaid targeted case management services include:
- “Comprehensive assessment and periodic reassessment of individual needs, to determine the need for any medical, educational, social, or other services;
- Development (and periodic revision) of a specific person-centered care plan based on the information collected through the assessment;
- Referral and related activities (such as scheduling appointments for the individual) to help the eligible individual obtain needed services, including activities that help link the individual with medical, social, and educational providers or other programs and services that are capable of providing needed services to address identified needs and achieve goals specified in the care plan; and
- Monitoring and follow-up activities, including activities and contacts that are necessary to ensure that the care plan is effectively implemented and adequately addresses the needs of the eligible individual and which may be with the individual, family members, service providers, or other entities or individuals and conducted as frequently as necessary, and including at least one annual monitoring.”
- Targeted case management referrals should be designed to assist eligible juveniles in connecting with services and providers – including services for health-related social needs – “in the geographic area where the eligible juvenile will be residing upon release, whenever possible.”
- If the state needs to transition the eligible juvenile to a new case manager upon release or after the 30-day post-release window, states should ensure a warm handoff, including: 1) a meeting between the eligible juvenile and both case managers; and 2) a review of the person-centered care plan and steps to ensure continuity of care.
- In CHIP, states must provide case management services “to the extent they are otherwise available under the CHIP state plan (or waiver of such plan) to children who are within 30 days of release.”
- CMS clarifies that Medicaid targeted case management services include:
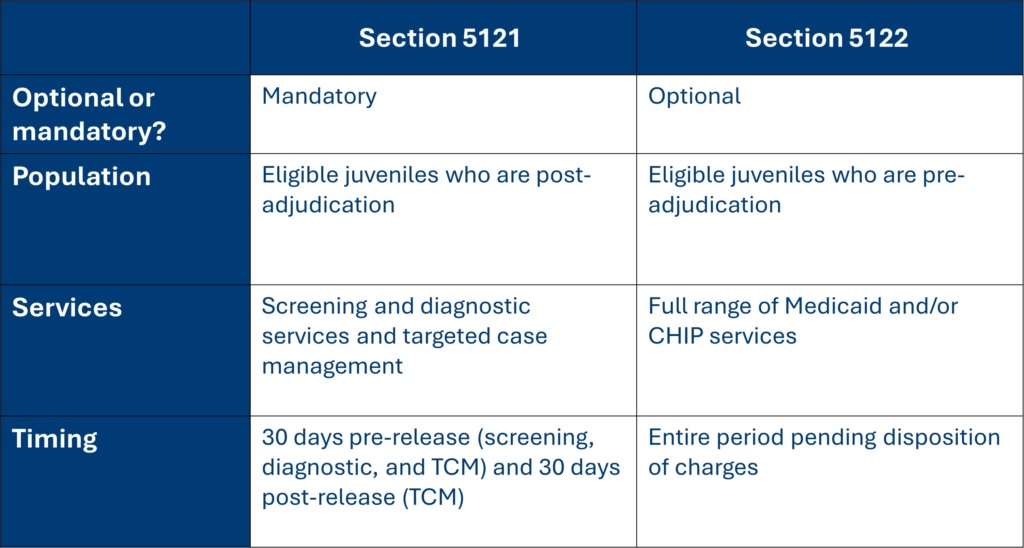
When do these services need to be provided?
Under Section 5121, states must provide screening and diagnostic services in the 30 days prior to release (or within one week or as soon as practicable post-release) and offer targeted case management 30 days prior to release and for at least 30 days post-release.
- If an eligible juvenile is screened prior to 30 days before their scheduled release – such as during intake or at another point during their incarceration – the state should evaluate if these services align with the state’s EPSDT requirements or other established standards for screening and diagnostic services. If they align with the state’s EPSDT standards (or other established standards), then the Medicaid agency can consider the Section 5121 screening and diagnostic services requirement satisfied.
- These same timeframes apply to CHIP. CMS reminds states that children are entitled to the full array of CHIP state plan benefits upon release.
- Scheduled release dates often change. If a release date is adjusted so that the eligible juvenile is no longer within 30 days of release, Medicaid agencies should “suspend coverage” of the required services until the eligible juvenile is within 30 days of the new release date. For CHIP, states may either suspend coverage or continue to provide CHIP state plan services not otherwise covered by the facility until the juvenile is within 30 days of the new release date.
Under the option at Section 5122, states would provide services for the full period of incarceration pending disposition of charges.
Which young people will receive these services?
The requirement at Section 5121 and the option at Section 5122 both apply to “eligible juveniles.” CMS defines eligible juvenile as “an individual who is under 21 years of age who was determined eligible for any Medicaid eligibility group, or an individual determined eligible for the mandatory eligibility group for former foster care children, immediately before becoming an inmate of a public institution or while an inmate of a public institution.” The mandatory eligibility group for former foster care children can include individuals up to age 26.
- The Section 5121 requirements only apply to eligible juveniles who are incarcerated “post adjudication.” CMS defines adjudication as “the court process that determines if an individual committed the act for which they are charged.” Thus, the Section 5121 requirements “apply where the court process has determined that the eligible juvenile committed the charged act and the court ordered the eligible juvenile held as an inmate of a public institution as part of the disposition of the charges.”
- Conversely, the option at Section 5122 only applies to individuals who are pending disposition of charges. CMS defines “pending disposition of charges” as meaning that “the eligible juvenile has been charged and is an inmate of a public institution while awaiting the outcome of the charges.”
What correctional facilities will be impacted by these requirements?
CMS says that the requirements apply to “all types of carceral facilities where an eligible juvenile post adjudication may be confined as an inmate of a public institution,” including state prisons, local jails, Tribal jails and prisons, and all juvenile detention and youth correctional facilities.
How can states take up the option at Section 5122?
Section 5122 allows states to provide coverage of full Medicaid and CHIP benefits for eligible juveniles who are pending disposition of charges. CMS defines “pending disposition of charges” as meaning that “the eligible juvenile has been charged and is an inmate of a public institution while awaiting the outcome of the charges.”
- Section 5122 allows states to lift the Medicaid inmate payment and CHIP eligibility exclusions for eligible juveniles who are incarcerated and pending disposition of charges. Under 5122, a state must provide all eligible juveniles with coverage of the Medicaid and/or CHIP services to which the juvenile would be entitled if not for their incarceration. This includes all mandatory and optional services to which they would otherwise be entitled, if not for their incarceration, including state plan services, waivers, and/or Section 1115 demonstration projects. For EPSDT-eligible Medicaid members, this also includes all EPSDT services.
- States may elect the Section 5122 option for Medicaid, CHIP, or both.
- Section 5122 would apply to the same carceral settings as Section 5121: any type of state prison, local jail, tribal jail and prisons, and all juvenile detention and youth correctional facilities.
- To implement this option, states would submit a Medicaid and/or CHIP SPA with an effective date no earlier than January 1, 2025. CMS is developing a SPA template.
What providers can states use to deliver the required services? How can states reimburse these providers?
In the guidance, CMS recommends that states use community-based providers to deliver the required pre-release services, as this may strengthen connections to the community upon release. However, CMS recognizes the operational challenges associated with building networks of community providers to deliver in-reach services, so states may use community-based providers or carceral health care providers. If a state uses carceral health care providers, these providers must comply with Medicaid and CHIP provider participation and enrollment requirements.
- States can use in-person or telehealth modalities to provide the case management, screening, and diagnostic services required under Section 5121. If Medicaid and CHIP agencies use telehealth, they should “collaborate with correctional entities to ensure the availability of appropriate technology that may be needed for health care services that are delivered via telehealth, as well as procedures to ensure appropriate privacy during telehealth visits.”
- All providers who will be “furnishing, ordering, referring, and rendering services” must enroll in Medicaid “if they are of a provider type that the state recognizes as eligible to enroll in Medicaid and CHIP.” Providers can either bill directly for services or “reassign their right to payment to the carceral facility or an agency contracted by the carceral facility to provide Medicaid-covered services.”
- States can use a fee-for-service or managed care delivery system to reimburse providers. States using managed care may need to modify their plan contracts and rates. CMS notes that, given the limited services delivered under Section 5121 and the differing acuity of this population, states should develop separate capitation rates for the “incarcerated eligible juveniles” group.
How do these requirements interact with Medicaid and CHIP eligibility policy? How does the Consolidated Appropriations Act of 2023 change CHIP eligibility policy?
Per the SUPPORT Act of 2018, states must suspend, not terminate, Medicaid eligibility for eligible juveniles who are incarcerated. States are also required to accept Medicaid applications from, or on behalf of, people who are incarcerated and process these applications timely. Finally, states are required to redetermine eligibility for certain incarcerated young people prior to their release from incarceration. The CAA made changes to CHIP eligibility policy to align with these SUPPORT Act requirements. In the guidance, CMS discusses these changes and clarifies how incarceration status interacts with continuous eligibility requirements in Medicaid and CHIP.
- As of January 1, 2025, states “may no longer terminate otherwise-eligible children from CHIP at renewal if the only reason for the termination is that they are inmates of a public institution.” To effectuate this, states may either suspend CHIP coverage (through a benefits suspension or an eligibility suspension) or provide all CHIP-covered services not otherwise paid for by the carceral setting.
- Young people up to age 19 must receive 12-month continuous eligibility for Medicaid and CHIP. Under CHIP regulations, incarcerated children are generally ineligible for separate CHIP. However, if a child is incarcerated during a continuous eligibility (CE) period, they must remain eligible for the duration of their continuous eligibility period. As of January 1, 2025, “states will no longer be permitted to terminate a child at the end of their CE period if they are still incarcerated.” To effectuate this, states may either suspend CHIP coverage or provide all CHIP-covered services not otherwise paid for by the carceral setting at the end of the continuous eligibility period.
- States must complete redeterminations for CHIP prior to release under certain circumstances. CMS also clarifies how Medicaid and CHIP redeterminations prior to release intersect with continuous eligibility.
- If a child is released before the end of their continuous eligibility period, the state must reinstate benefits without conducting a redetermination of eligibility (unless they have experienced an exception to continuous eligibility, like turning 19).
- If a child is released after their continuous eligibility period ends and the state has not completed a redetermination in the last 12 months, the state must complete a redetermination prior to release.
- For eligible juveniles who are not eligible for continuous eligibility (such as kids aged 19 or older), the state must redetermine eligibility prior to release unless the last redetermination occurred after individual was incarcerated and within 12 months of the date of release. This policy is described in detail in January 2021 guidance on the SUPPORT Act.
- Under Section 5121 of the CAA, children who apply for CHIP coverage within 30 days of release may be found eligible for the required screening and diagnostic services, referrals, and case management services. States must process applications for full CHIP benefits upon release.
How do data sharing laws apply?
CMS notes that multiple laws and regulations may impact data sharing across health care and correctional systems, including “section 1902(a)(7) of the Act, discussed in further detail below; 42 C.F.R. Part 431, Subpart F; 42 C.F.R § 457.1110; 42 C.F.R. Part 2;63F 64 and the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy, Security, Breach Notification, and Enforcement Rules (the HIPAA Rules) as well as state-level regulatory requirements.”
42 C.F.R. part 431, subpart F requires that Medicaid agencies provide safeguards around Medicaid member and applicant data, including obtaining permission before making a data disclosure to an outside source. CMS clarifies that an entity “such as [an] enrolled carceral health care provider who is contracted to assist the agency in a purpose directly connected to the administration of the Medicaid or CHIP state plan, such as providing services to beneficiaries, would not be considered an outside source” for the purposes of 42 C.F.R. part 431.
What does CMS recommend in terms of implementation?
- CMS notes that it may be difficult to identify former foster care youth who are eligible for Medicaid, as corrections staff generally do not collect data on former foster care status. CMS states that “identifying this population may require individual surveys of young people” and that “Medicaid agencies will need to determine a mechanism to identify former foster care youth, and then assess their Medicaid coverage status, notifying the adult facility of their eligibility as applicable.”
- To ensure access to services for potentially eligible individuals, CMS states that Medicaid agencies “should work with their correctional facility partners to establish procedures to start the application process, and assist incarcerated youth who are not already enrolled in Medicaid with applying for Medicaid upon incarceration and during the period of incarceration, with a goal of application submission no later than 90 days before the individual’s expected date of release to allow for application processing time.” CMS notes that, although state laws vary on who may sign a document on a minor’s behalf, “42 C.F.R. § 435.907(a) allows someone ‘acting responsibly’ to sign and submit an application on behalf of a minor who is incarcerated.”
- CMS recommends that state Medicaid and CHIP agencies engage justice system entities to establish data sharing agreements.
- CMS encourages states to expand the availability and utilization of peer support services for youth who are reentering from incarceration.
States must ensure compliance with Medicaid and CHIP requirements on accessibility for individuals with limited English proficiency and/or disabilities.
Related resources
How Medicaid Provider Taxes Work: An Explainer
Why Did They Do It That Way? Program Integrity
Stay Informed
Drop us your email and we’ll keep you up-to-date on Medicaid issues.