The Phases of Unwinding: A Framework for the End of Continuous Coverage
This blog outlines NAMD’s framework to break down the unwinding of the public health emergency into three distinct phases and to help the program’s partners anticipate the arc of this effort.
The nation’s Medicaid program is about to embark on a major undertaking: redetermining eligibility for all 90 million people on the program and returning to normal eligibility operations. Medicaid’s partners, including policymakers, health plans, providers, community-based organizations and others will play a critical role in this work. Knowing where we are – and where we’re headed – in this effort is important, especially for Medicaid’s partners. That’s why NAMD developed a framework to break down the unwinding into three distinct phases and to help the program’s partners anticipate the arc of this effort.
The context for Medicaid’s unwinding Before we dig into the unwinding framework, it is important to ground ourselves in what this effort is and why it is happening.
During the pandemic, Medicaid programs in all states, DC and the territories have been a vital means of ensuring access to health care for low-income seniors, people with disabilities, families, working adults and children. Not only did Medicaid cover COVID-19 testing and vaccines, but it pivoted to allow people to get many types of medical and behavioral health care through accessible means.
When the pandemic started, Congress enacted a federal requirement that states and territories continue to cover every person who became eligible for Medicaid until the public health emergency was lifted, even if their income or other circumstances changed – the so-called “continuous coverage” requirement. Recognizing the progress that the country has made in responding to the pandemic, however, in December 2022, Congress authorized states, DC and the territories to begin the process of redetermining the eligibility of all people on the program.
This big undertaking – the “unwinding” process – started in February 2023 and will continue for over the next 14 months, depending on when a state starts its unwinding period. Medicaid agencies remain committed over this time to:
- Observing normal procedural requirements for eligibility redeterminations;
- Paying special attention to people who are the most likely to be disconnected from the health care system; and
- Complying with all federal requirements for unwinding.
With more than 90 million individuals counted as Medicaid members, this is the largest undertaking of its kind by the program. (For more background about unwinding, check out this blog.)
A framework for unwinding This work is now underway, and Medicaid and its partners are in the trenches. This framework is designed to help us lift up and see the work ahead. It breaks down the unwinding effort into three distinct phases:
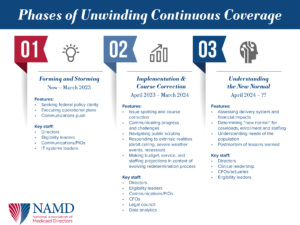
Phase 1: forming and storming – a period characterized by final preparations to begin the work of redeterminations.
Phase 2: implementation and course correction – a period characterized by rapid learning, ensuring warm handoffs to other coverage, and responding to unanticipated challenges.
Phase 3: understanding the new normal – a period characterized by assessment and response to how unwinding has changed Medicaid and the health care delivery system.
Let’s dig into each of these phases in detail.
Phase 1: forming and storming This is the phase we are in now. Medicaid programs are getting ready for, and some have already started, activating their unwinding operational plans – plans that were in development for many, many months. As the starting gun goes off, Medicaid leaders are continuing to work with the program’s federal partners at CMS to get clarity on the rules of the road that Congress outlined in the Consolidated Appropriations Act, 2023. This includes clarity around new compliance expectations, and what exactly it means for states to reach out to members through multiple modalities (e.g., phone, email, text messaging) when mail is returned unopened.
There’s also a big communications push happening. Not only are notices starting to go out, but states are launching communications campaigns to let members what action to take and when. Many states have also been running campaigns to encourage members to keep their addresses updated and respond to agency requests for nearly a year. Medicaid Directors, eligibility leaders, and communications leaders are on the frontlines. But perhaps the unsung heroes, back behind the scenes, are the IT systems leaders. They are pivoting and responding to CMS guidance to get systems ready and doing so much more quickly than normal. This includes making sure their systems are configured to support new federal policies around returned mail. IT leaders are also running systems tests to make sure all-systems-are-go.
Phase 2: implementation and course correction This phase gets into full swing sometime in late spring and will run through first part of next year. Think of this as the first quarter of a game. Medicaid leaders will be knees bent, on the field, ready to respond when issues inevitably arise. They will be asking, “Where is our strategy working? Where is it not working? Where do we need to pivot?”
Data will be critical in this phase. Medicaid leaders (especially data analytics staff), the federal government, and policymakers will be monitoring metrics and trends to quickly spot and respond to concerns. Some of these metrics include the number of people who retain their Medicaid coverage, the number of individuals who have their coverage terminated for procedural reasons, and the volume of calls coming into state call centers. Medicaid programs have lots of experience monitoring metrics like this and doing rapid-cycle-learning, including in the early days of the COVID-19 pandemic and during Affordable Care Act implementation.
There is also going to be a lot of public attention on Medicaid. Partners, policymakers, and stakeholders will also be eager to understand how it’s going. They will be focused on federally-reported metrics and on the public-facing dashboards that some states have opted to create.
In addition, Medicaid programs will be focused on ensuring warm handoffs to other sources of affordable coverage for those who are no longer eligible for the program. They will connect these individuals to the federally-facilitated or state-based marketplace, which will then determine if these individuals are eligible for subsidized commercial coverage. For children, Medicaid programs will also make warm handoffs to the Children’s Health Insurance Program, or CHIP, in states that administer a separate CHIP program.
Finally, Medicaid programs will still need to execute other core functions of the program in this phase, but with uncertainty looming large. These are things like budget development, updating capitation rates, issuing requests for proposals, making service projections, and implementing other state and federal policies. All of these efforts will be impacted by evolving projections and the many ripple effects of unwinding.
Phase 3: understanding the new normal This is, perhaps, the most complex and difficult phase, and it could last the longest. Medicaid agency leaders will have to assess how unwinding has fundamentally changed the program and what the new normal is. For instance, it could take months or years after redeterminations are complete to understand new enrollment trends and how many people Medicaid will continue to cover ongoing. Medicaid leaders will have to use the best available data to make these estimates and continuously adjust financial forecasts.
In addition, programs will have to assess how unwinding has changed the needs of Medicaid members. For instance, long-COVID, a greater preference for home- and community-based options for long-term care, and more prevalent behavioral health conditions are just three ways in which Medicaid members’ needs will likely evolve. Understanding these changes will be critical for all aspects of program administration, from benefit design to financial forecasting.
Finally, we know the impacts on the delivery system could be significant. The Urban Institute estimates that as many as 18 million people may transition off Medicaid insurance coverage. Almost four million of those individuals may be uninsured and disconnected from the health care system. This could put additional pressure on safety-net providers, like federally-qualified health centers and rural hospitals, which serve uninsured individuals and are also a core component of the delivery system that serves all Medicaid members. Understanding these new realities will take time, data, analysis and strategic leadership across Medicaid and the health care delivery system as a whole.
A few concluding thoughts As Medicaid programs and its partners jump into the work of unwinding, it’s easy to get lost in the sea of policy issues, questions, and operational details. Contemplating the road ahead as three distinct phases — forming and storming, implementation and course correction, and understanding the new normal – can help the program’s partners best engage with and support Medicaid programs in this effort.
Related resources
How eligibility may look different in this bridging year
NAMD Comments on CMS’s Interim Final Rule on the Medicaid Unwinding
Stay Informed
Drop us your email and we’ll keep you up-to-date on Medicaid issues.