What We Know About Medicaid and Who it Serves
A look at who Medicaid serves today and how the program serves those members
Author
- NAMD
Focus Areas
Program Stream
Project

In late March, the Kaiser Family Foundation published their public opinion poll on the Medicaid program. More recently, the Center for Medicare & Medicaid Services (CMS) released the 2023 Medicaid and CHIP Beneficiary Profile outlining enrollment, characteristics, health status, and the experience of Medicaid and Children’s Health Insurance Program (CHIP) members.
For the past three years, states have been required to keep members continuously enrolled in insurance through the Medicaid program. Because of this continuous coverage requirement, Medicaid now covers over one in four Americans. Medicaid primarily covers children, pregnant people and older adults as well as some other adults who have lower incomes as well as individuals with disabilities.
As states are beginning the process of resuming normal eligibility operations, here’s a look at who Medicaid serves today and how the program serves those members.
Who does Medicaid serve?
Nearly sixty percent of adults say that either a family member, a close friend, or they themselves have been a Medicaid member in their lifetime. The program’s reach extends beyond 90 million individuals today. Medicaid specifically provides coverage for three major populations including:
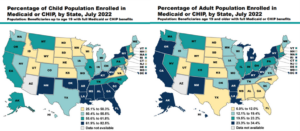
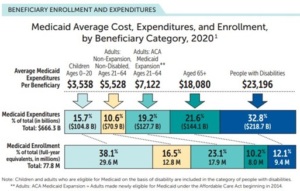
- Families and children: Nearly four in ten children in the United States are covered by the Medicaid program. Coverage penetration ranges from 25.1 percent to 82.5 percent of children across states. The plurality of Medicaid members are children, comprising 38 percent of the total Medicaid membership today. Moreover, 16.5 percent of Medicaid members are non-expansion, non-disabled adults. This may include pregnant people, very-low income caretakers and adults, along with some former foster care adults, further exemplifying Medicaid’s role in supporting families.
- Older adults and people with disabilities: Older adults and people with disabilities, together, make up 22 percent of the total Medicaid membership yet, they account for over half of the total expenditures in the program. This is largely because of their higher health care and social needs.
- Low-income adults: Medicaid also plays a significant role in covering low-income adults who do not have access to other sources of health care coverage. Since the passage of the Patient Protection and Affordable Care Act (ACA), states could expand Medicaid eligibility for low-income adults up to 138 percent of the federal poverty line. With 38 states and the District of Columbia adopting and implementing this expansion, 23.1 percent of Medicaid members are ACA expansion adults.
Medicaid members also tend to reflect characteristics of the broader population of their state. For instance, 60.1 percent to 67.9 percent of Medicaid members live in rural areas in some of the most rural and frontier states.
The program also plays an outsized role in covering Black or African American and Hispanic or Latinx children and adults. In 2021, 42 percent of Medicaid members were White, 28 percent were Hispanic or Latinx, and 18 percent were Black or African American.
What are Medicaid members’ health and health-related needs?
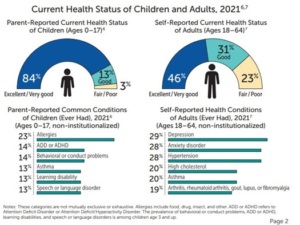
Health-related needs can vary among cohorts of Medicaid members. For instance, more than 8 out of ten parents reported that their Medicaid-enrolled child was either in excellent or very good health. Meanwhile, only 46 percent of adult Medicaid members indicated that they were in excellent or very good health. Medicaid members have distinct needs in the following areas:
- Behavioral Health: Nearly one in three Medicaid enrolled children have a mental, emotional, developmental, or a behavioral need. Depression and anxiety are the most reported health conditions among adults.
- Maternal Health: Medicaid covers over 2 in 5 births in the United States. This can range from 21.7 percent of births to 60.8 percent of births across states. The incidence of births to women served by Medicaid is on the high end of this range in economically distressed areas.
- Long-term Care: Because of its role covering individuals with disabilities and older adults, Medicaid is the single largest payer of long-term care in the country, which includes services provided at a nursing facility and home and community-based services.
- Chronic Conditions: Medicaid’s coverage of key preventative medical and behavioral health care plays a vital role in supporting individuals in managing their chronic conditions. For instance, 20 percent of adults and 13 percent of children enrolled on Medicaid have asthma. Other common conditions among adult Medicaid members include hypertension, high cholesterol, and arthritis.
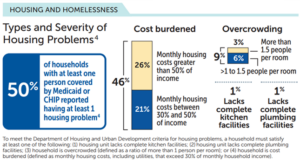
Because of its role covering individuals with lower incomes, Medicaid members have higher social needs. For instance, half of Medicaid households reported at least one housing problem, notably, around high housing costs. Nationally, 24 percent of children and 30 percent of adults on Medicaid experienced either low/very low food security or marginal food security.
How does the American public view the program?
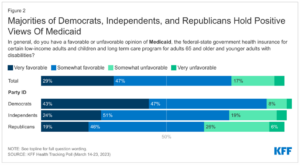
Generally, Medicaid members and the American public at-large view the Medicaid program positively. More than two out of three people say that the Medicaid program is working well for most low-income people covered by the program, and 76 percent of Americans hold a positive view of Medicaid.
Related resources
The Impact of Medicaid on the Rural Health Care Landscape
Stay Informed
Drop us your email and we’ll keep you up-to-date on Medicaid issues.